Tasha
“I'm too functional to be disabled, and I'm too disabled to be functional.”
MILFORD, CONNECTICUT: I work at a physical therapy and orthopedic office. When the pandemic hit, they gave us one mask each. Since there was a shortage of PPE kits, we were allowed to wear the mask only if the patient came in symptomatic. We screened patients, but all weren't honest. They would say they didn't have any symptoms and then cough non-stop in the waiting room. At that time, we did not know exactly how it spread. We had people in the waiting room coughing and sneezing. I went out there every hour with wipes and gloves on, no mask, and cleaned down the chairs, the tables, the door handles, the bathrooms, and push plates to keep everyone safe.
We screened patients, but all weren't honest. They would say they didn't have any symptoms and then cough non-stop in the waiting room.
I'm not sure where I got sick, but the diarrhea started a good week before I tested positive and before the other symptoms. Early on, diarrhea wasn't a Covid-19 symptom. My husband tested positive on April 1st, I had already had diarrhea for a week, so I don't know who caught it first. He's a carpenter and goes into empty houses damaged by fire or water to remodel them but he wasn't around people.
I thought it was my nerves with the whole pandemic. Then I woke up on my 40th birthday, April 4th, with a nasty smell in my nose, and it was all I could smell. I asked everybody if they could smell it, but nobody else could. I also couldn't go outside without my sunglasses on. The sun bothered my eyes; it was too bright. Then over the next few days, I started to have a sore throat, a cough, body aches, and intense headaches.
I tested positive on April 8th.
The third or fourth week, I went to walk up my front steps, and I had to pull myself up the stairs. I went to the emergency room to be checked out. The PA told me she didn't want to have COVID blinders, and any neurological condition can cause leg weakness, pain, and trouble with stairs. I said, “In 40 years, I've never had trouble walking. I've been able to do stairs. So I'm pretty sure that COVID caused it.” But, they only did blood work, gave me one quick bag of fluids, and sent me on my way. They didn’t even listen to my lungs. It was a waste of time. It made me feel abandoned.
The first four to five weeks, I had a cough and a burning pain in my chest. It felt like somebody was stabbing me with little needles in my lungs. I also had shortness of breath, body aches, muscle weakness, and headaches. But, I thought I was getting better.
It felt like somebody was stabbing me with little needles in my lungs.
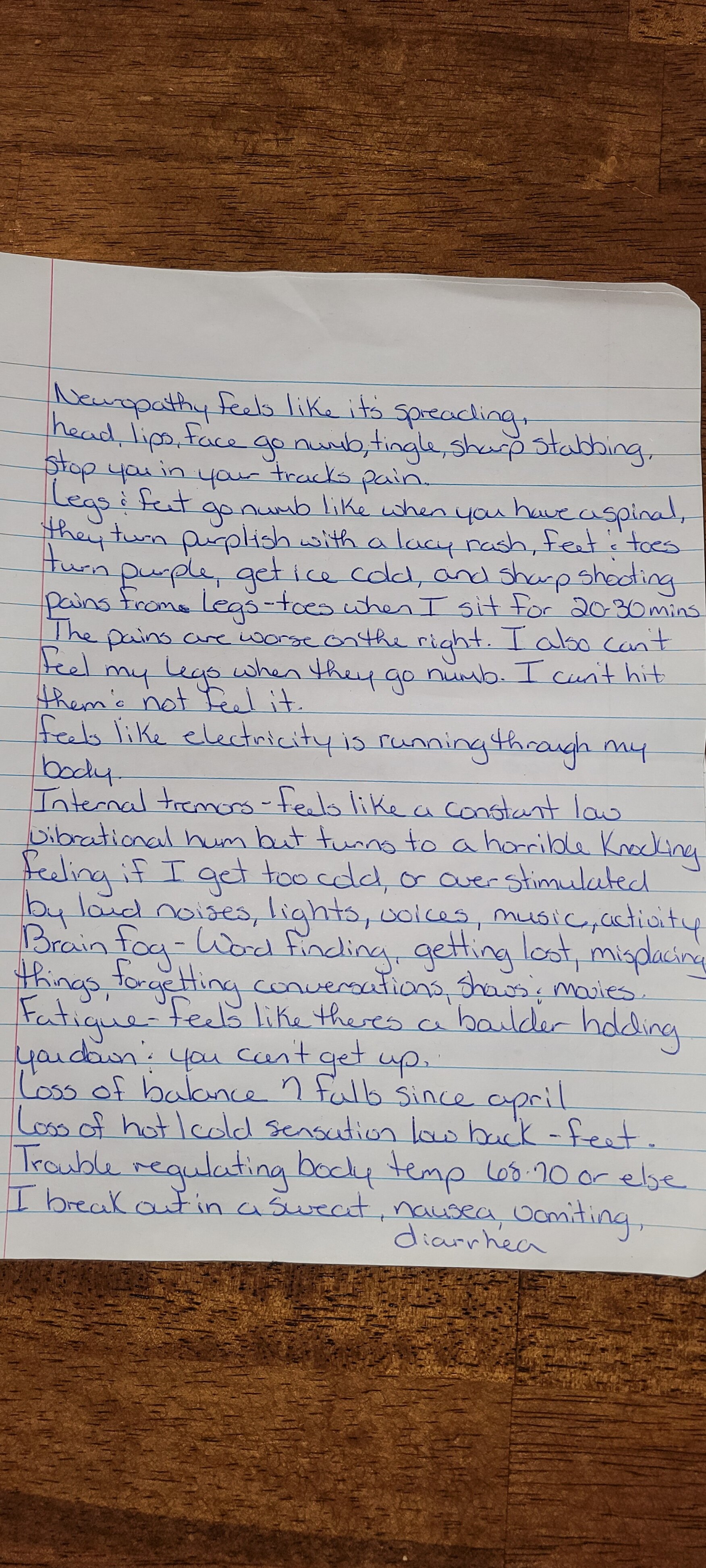
Around week six, more neurological symptoms started: numbness, tingling, and burning in my legs and my feet. It has since moved to my hands, arms, and head. My face gets numb and tingles now as well. I've developed stabbing, shooting pain in my face and my head. It stops me in my tracks it's so intense. I've been having a lot of muscle spasms and foot cramps that keep me up at night. It’s hard to get comfortable when your skin feels like someone is holding a blow torch to it, and you feel like you have something crawling all over you. Then my muscles start spasming. Some nights my feet burn so bad I go outside and put them on the ice-cold pavement or in the snow. My hands feel swollen. It hurts to bend them, and they feel very tight like they might snap, but they're not swollen. I also don't have any hot or cold sensation in the lower half of my body. My legs go numb, and it feels like I’m going to fall and need to sit down. I have fallen seven times since I had COVID and sprained my ankle once. My legs always feel tired and weak, like the day after a really bad charlie horse. I have internal tremors that feel like there is a cell phone vibrating in my body; it goes from a vibrating to a knocking feeling. My body has a hard time regulating temperature. I get overheated easily, which causes me to break out in a sweat and have vomiting and diarrhea. I get overstimulated with bright lights and loud noises. My heart rate and blood pressure fluctuate. I can't sit in a chair for more than 20-30 mins, or else my legs and feet get a purple lacy rash on them. My toenails turn purple. My legs and feet get ice cold and go numb along with shooting, stabbing pains down to my toes.
It’s hard to get comfortable when your skin feels like someone is holding a blow torch to it
I feel like I'm getting worse. I'm getting more symptoms. The pain is back in my lungs. If I overdo it, I will be in bed for two to three days. My resting heart rate is about 56, but it shoots up into the hundreds when I stand up. When I take a shower, my heart rate is 120's-150's. It drops down as low as 30. I have memory issues, word-finding difficulty, and trouble concentrating.
If I overdo it, I will be in bed for two to three days.
I was on 1800 milligrams of Gralise at night and 150 mg of Oxcarbazepine. It's supposed to help with the nerve pain, and it did in the beginning, but it wasn't helping anymore, so the doctors changed my medications to 150mg of Lyrica twice a day and doubled the dose of the Oxcarbazepine to 300 mg. I’ve had two rounds of IVIG and awaiting my next two.
My doctors don't have a clue what's going on. Nobody does. But they're trying. I've had a punch skin biopsy, a lumbar puncture, a CT scan of my lungs, and MRIs to try to get to the bottom of it. My lumbar puncture and my thigh biopsies were abnormal. That's why they thought I might have an autoimmune disease. No one has been able to give me any answers. They say they're still learning. They think that I might have dysautonomia or POTS (postural orthostatic tachycardia syndrome), Chronic fatigue syndrome, fibromyalgia, and/or ankylosing spondylitis but nobody has a clue. The diagnoses I've been given so far are peripheral polyneuropathy, paresthesias, disease due to severe acute respiratory syndrome coronavirus 2,and mild air trapping in my lungs. I'm hopeful that the doctors can figure out what's wrong with me. I want it to be nothing, but I almost want them to find something, give me a diagnosis, give me medicine to try to make it as good as we can so I can at least go back to work.
My doctors don't have a clue what's going on. Nobody does.
My employer accommodated my ADA request for two months which has allowed me to work from home. I just found out that it is ending, and I'm still unable to return to the office due to my health issues. I was told if I can't return to the office I need to look for to new job. I've been trying to work as much OT as I can in case I lose my job. I was out of work from April - December. I'm too functional to be disabled, and I'm too disabled to be functional. I feel like I'm in a grey area. I can work in a reclined or laying down position all day but put me vertical and forget it. I last maybe 30 minutes.
I'm too functional to be disabled, and I'm too disabled to be functional.
Tasha during a sleep study.
I had a sleep study on February 5, 2021. I've developed mild sleep apnea since Covid-19. He said the most important finding was long periods of sustained oxygen levels below 88%. He said, “I'm thinking about putting you on oxygen at night.” I started to cry. He said first he will bring me back in and do another sleep study with a CPAP machine to see if that helps the oxygen levels. If it does, I will need a CPAP. If it doesn't work, I'm going to need to go on oxygen at night at age 40.
He said the most important finding was long periods of sustained oxygen levels below 88%… If it doesn't work, I'm going to need to go on oxygen at night at age 40.
Before Covid, I'd get up for work around 6:30 AM, get ready for work and get the kids ready for school. I would go to work from 7:30 to 4 PM or 6 PM. I had up to 86 patients a day that I'd have to check-in and schedule appointments for plus answer the phones. Then I would go home, cook dinner, or my husband would have it done if it was a late work night, and I would clean up the house, do some laundry, and take the kids wherever they had to go. Or run to the grocery store, shower, go to bed, wake up and do it all over again.
On a typical day now, before I started back at work, I don't get up until 10 or 11 AM because I'm not falling asleep until 2 - 4 AM. When I get up, I don't do much. I'll maybe do some dishes and then rest. If I go grocery shopping, then I can't do anything else during the day. Sometimes I only eat one or two meals a day because nothing tastes good. I have a horrible metallic and sour taste in my mouth. My husband is currently on unemployment. We take turns making dinners, and sometimes we end up ordering something because neither one of us have the energy to cook. My girls are 12 and 10, so they help out sometimes. I can't even shower every day. It takes too much out of me. Sometimes I forget to take my meds or eat.
I can't even shower every day. It takes too much out of me.
There have been days where I feel like giving up. I've had some dark thoughts at times that have scared me. I’m so tired and in so much pain from the time I wake up to the time I fall asleep my skin feels like someone is holding a blowtorch to it, and I always feel like something is crawling on me. It makes for a rough day, and I never get full relief. I had two IVIG infusions three weeks ago, and they are hopeful it will help calm down my immune system. I'm also on a daily dose of Prednisone and have been since December.
Covid has turned my 12-year old into a long-hauler, which is terrifying and heartbreaking to see. She has horrible headaches, joint and muscle pain, mottled rash, and elevated heart rate,fatigue. Her hands and feet get ice cold and turn purplish. As of 2/19/21 she was started on preventative medicine for migraines.
People make jokes about the masks and don't want to be controlled by the government, but they don't realize what this could do to them. People are like, “Oh, I'm healthy. I have a good immune system. I'm going to be fine.” You go on Survivor Corps or Long-Haul COVID fighters, and you’ll find avid runners who ran marathons, people who worked out every day, fitness coaches. COVID doesn't discriminate. It doesn’t care if you're overweight and 40. It doesn’t care if you're skinny and you run every day and you only eat vegetables. It doesn't matter. You don't know how it's going to hit you until it does. That's what people aren't getting. It affects you physically and mentally, and if you end up being a long-hauler, it affects you financially. I've had to use almost everything I had in my savings to survive up to this point. I don't know what that's going to look like going forward. Will I be able to work, or will I become disabled? I REALLY can't become disabled. I would lose everything: my house, my car, our health insurance, and my life insurance. It affects your whole life, especially if you end up having it for more than two weeks. I've been sick for almost a year. I'm looking at a job change or a job loss. I was out of work for eight months. I've depleted everything I've worked so hard to save. Covid has taken so much from me.
COVID doesn't discriminate. It doesn’t care if you're overweight and 40. It doesn’t care if you're skinny and you run every day and you only eat vegetables. It doesn't matter. You don't know how it's going to hit you until it does.
It's terrifying because you don't know what the future holds because they don't know the disease. I don’t know if it will get better or worse or the same, and not having any answers makes it super, super stressful, and scary. You wake up one day, and your whole life changes. I keep waiting to wake up and have my health back, but it never happens. I know it happens to people all the time, and I've been through my share of things that have rocked my life. But, this is one of the worst things I've been through.
I don’t know if it will get better or worse or the same, and not having any answers makes it super, super stressful, and scary.
Tasha’s Advice:
Don't give up, keep fighting, if your doctors aren't taking you seriously find one who will. What you are experiencing is real and valid. Pace yourself and learn your limits so you don't end up in bed for days. You have to advocate for yourself and you need a good support system if you don't have that with your family or friends there are some great groups on Facebook or Instagram.
Tasha, 40, is a mother of two daughters, wife, and worked as a receptionist at a physical therapy and orthopedic office. She is currently enrolled at a post covid neurological research program at Yale.
Symptoms: diarrhea; sore throat; cough; body pain; headaches; hands and feet get ice cold; numbness and tingling in feet, legs, hands, and arms and sometimes face and head; fluctuations in blood pressure and heart rate; muscle spasms; eye pain and twitches; overstimulated easily with light and sound sensitivity; insomnia; mottled rash on legs; numbness if sitting for more than 20 - 30 minutes; legs always feel weak like the day after a bad charlie horse; internal tremors; shortness of breath.
Treatment: Z-Pack, Gralise 1800 mg, Oxcarbazepine 300 mg, Lyrica 150 mg, Prednisone daily, two IVIG infusions.
Post-Covid Diagnoses: peripheral polyneuropathy, paresthesias, disease due to severe acute respiratory syndrome coronavirus 2, myalgia, sleep apnea, dysautonomia, POTS
Blood Type: O Negative
Pre-Existing Conditions: mild childhood asthma